Understanding the Lumbar Dermatome Map: A Guide to Sensory Pathways and Diagnosis
Related Articles: Understanding the Lumbar Dermatome Map: A Guide to Sensory Pathways and Diagnosis
Introduction
In this auspicious occasion, we are delighted to delve into the intriguing topic related to Understanding the Lumbar Dermatome Map: A Guide to Sensory Pathways and Diagnosis. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Understanding the Lumbar Dermatome Map: A Guide to Sensory Pathways and Diagnosis
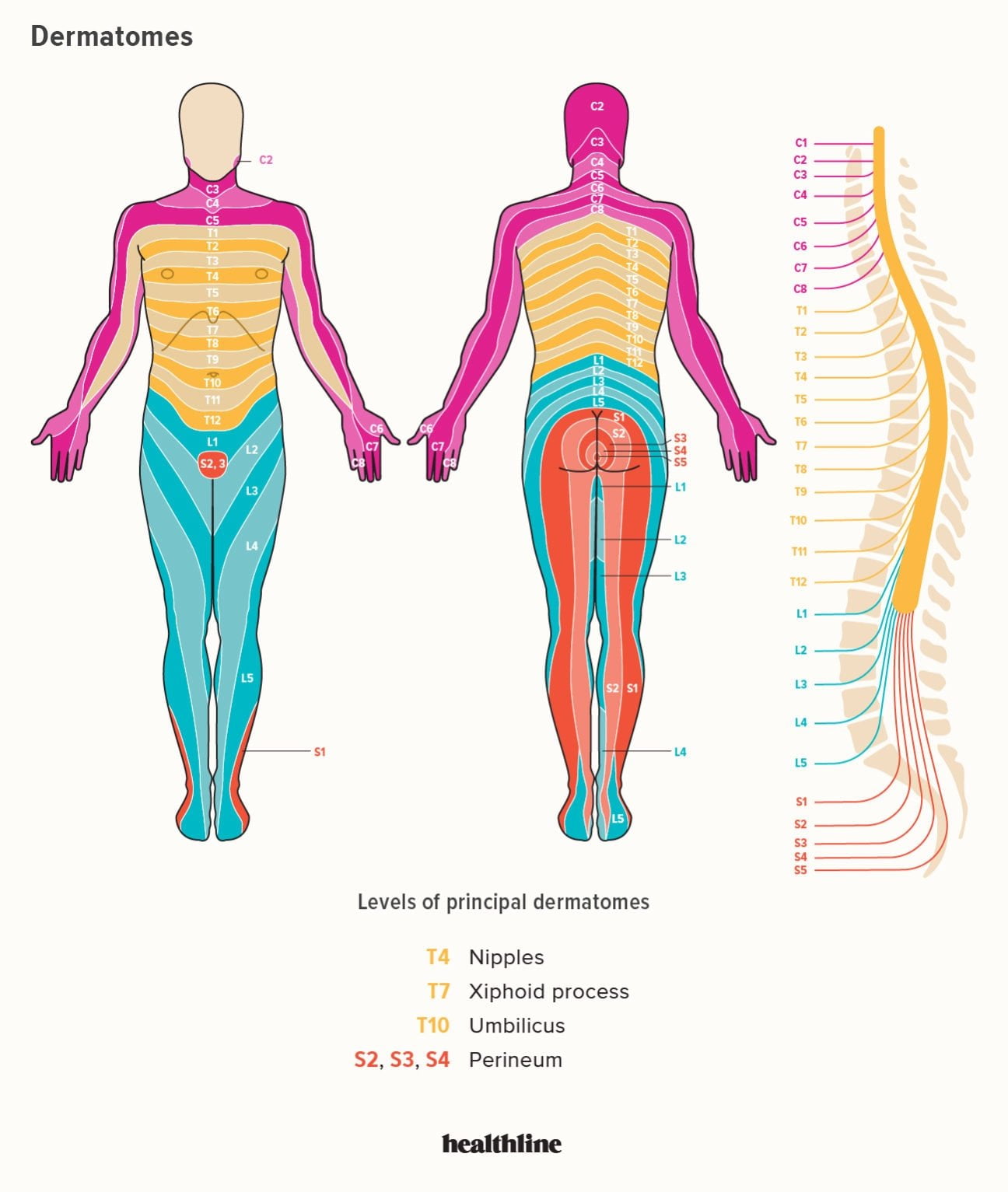
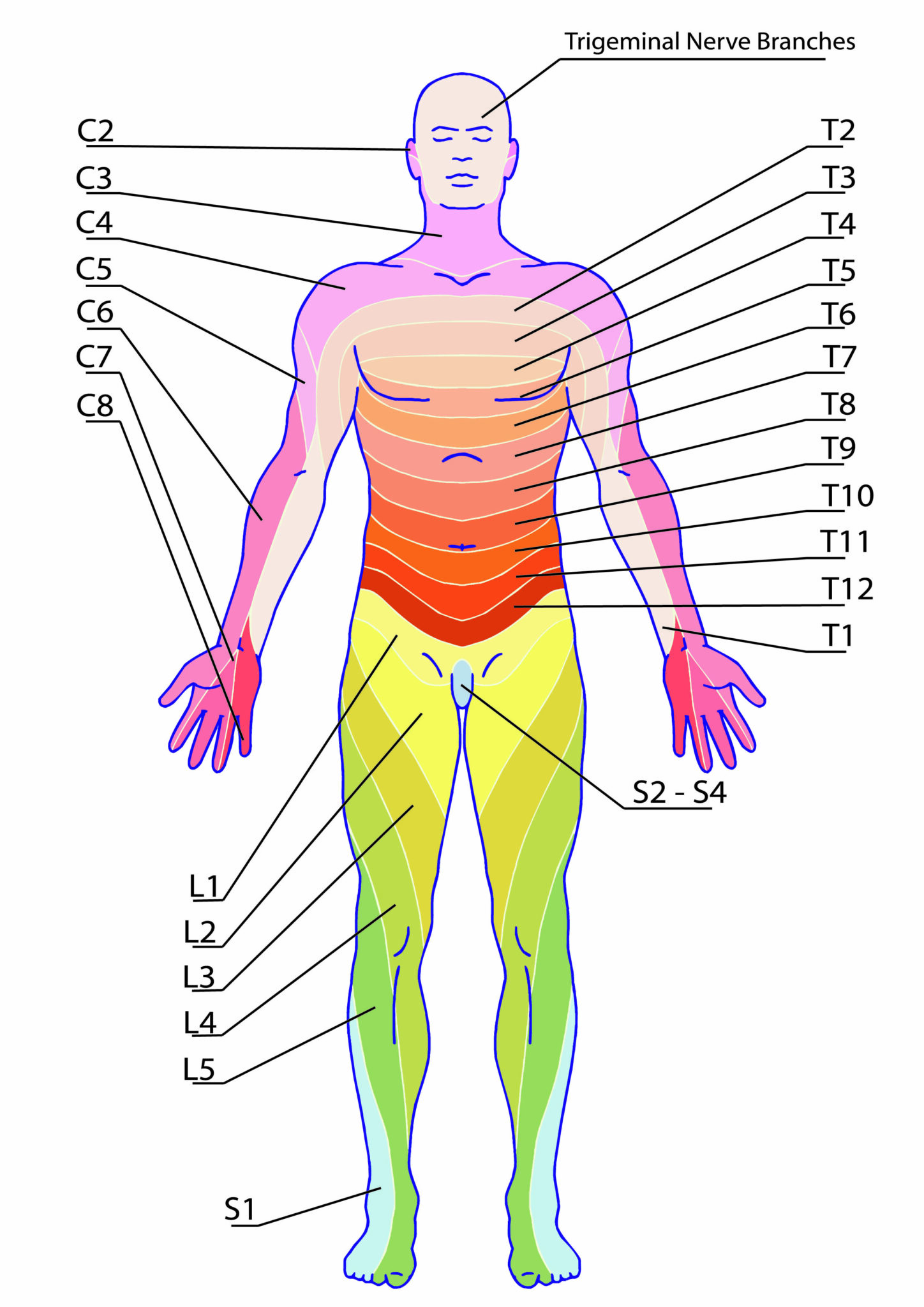
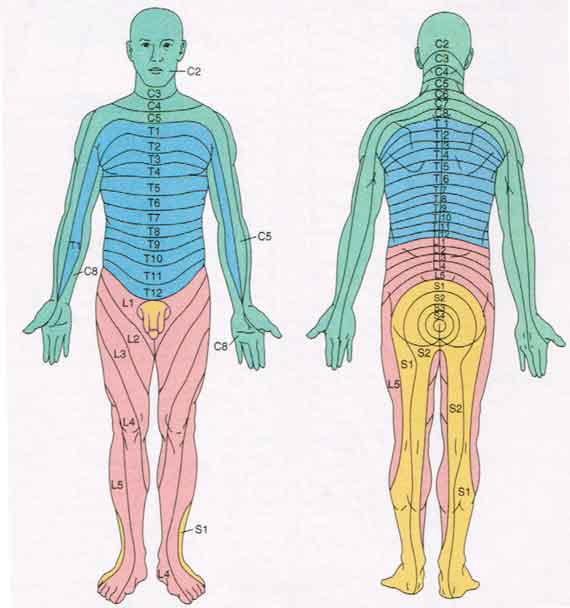
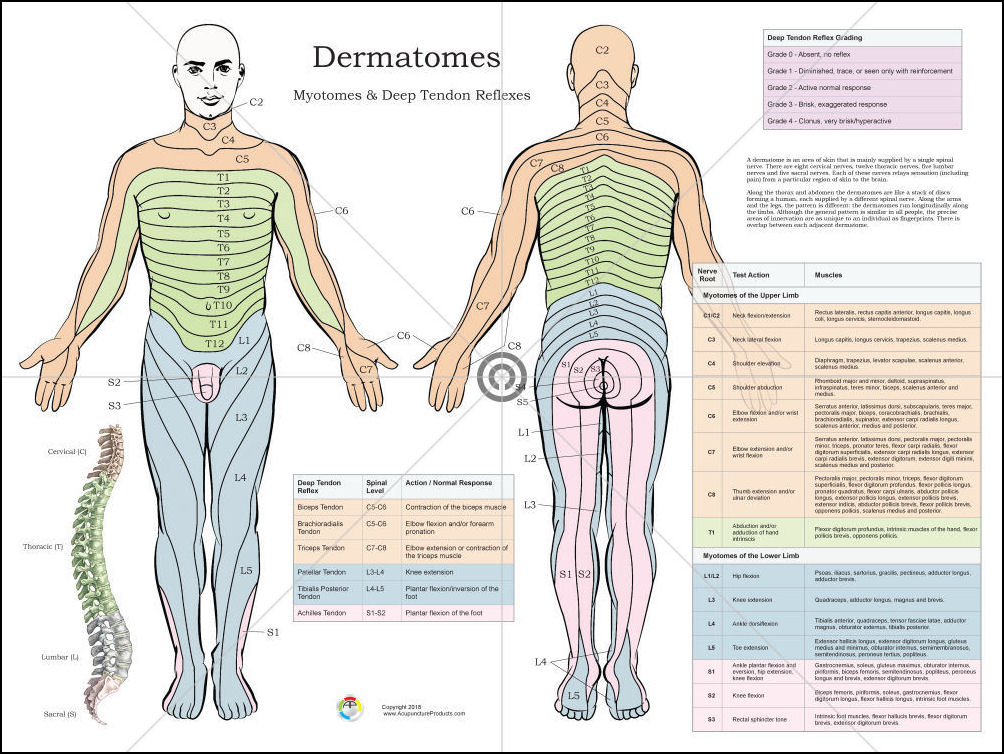
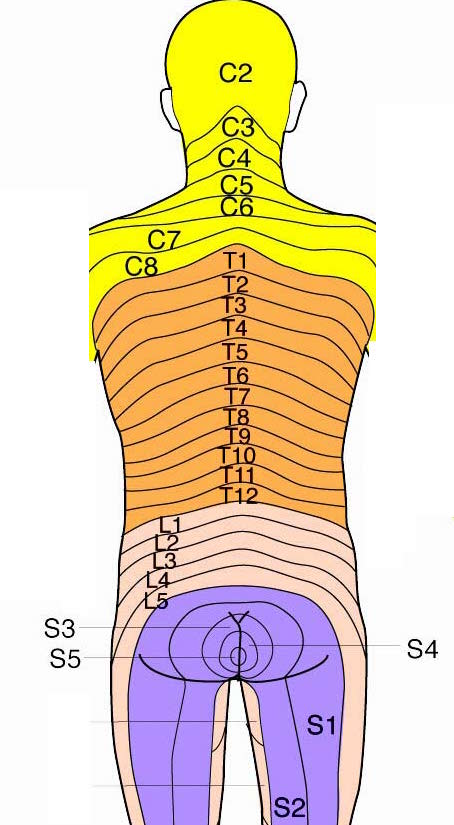
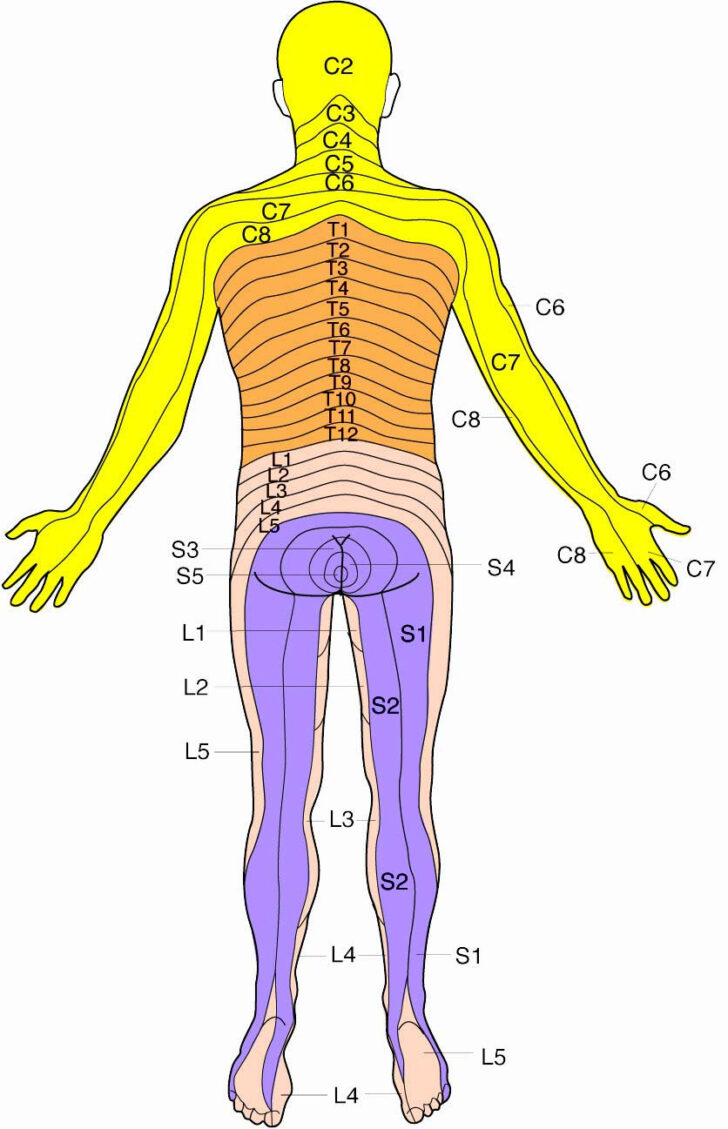
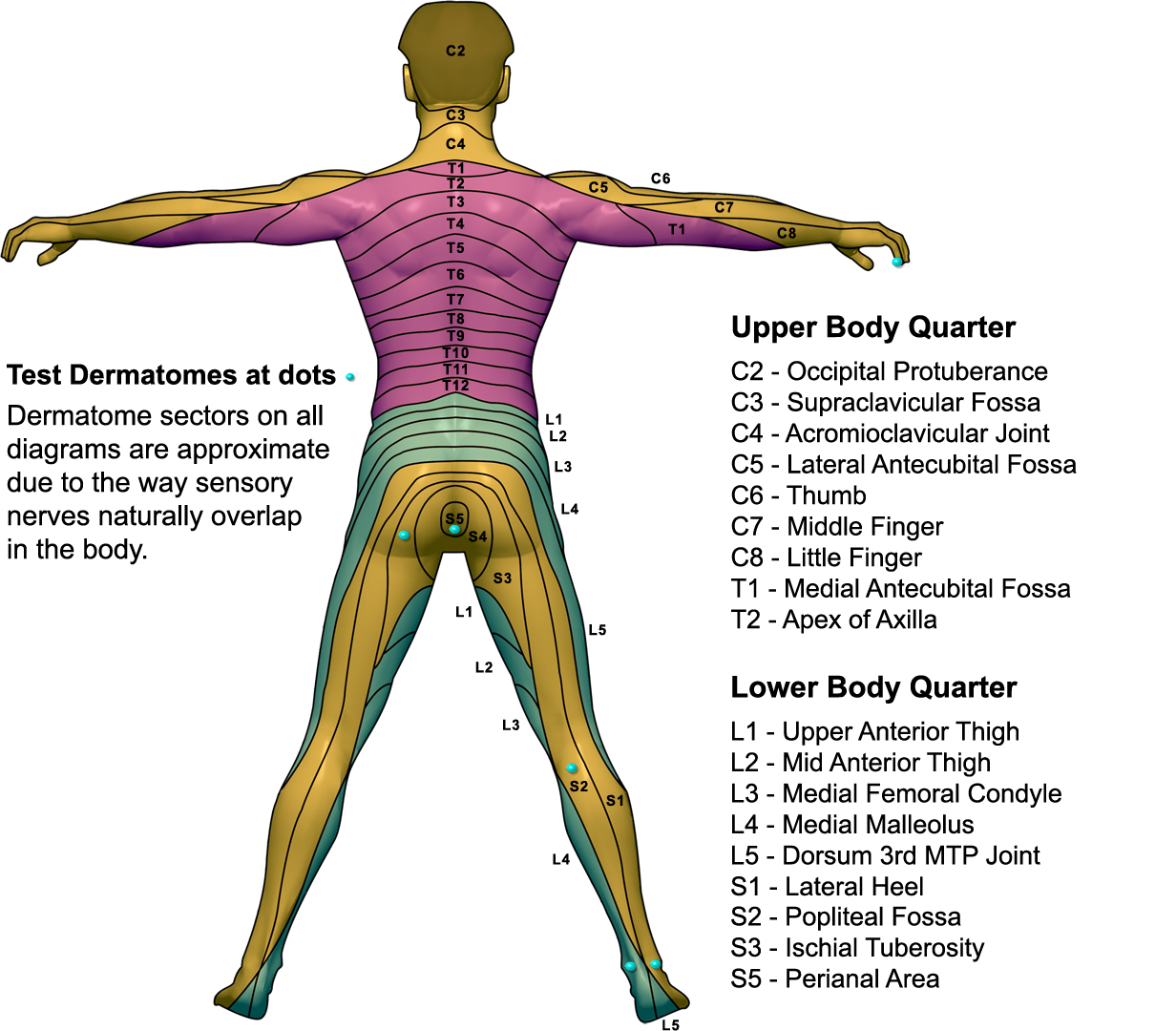
The human body is a complex network of interconnected systems, and understanding its intricate workings is essential for medical professionals. One such system, crucial for diagnosing and treating a variety of conditions, is the dermatome map. This map, a visual representation of the sensory innervation of the skin, is a vital tool for neurologists, physicians, and physical therapists.
Delving into the Dermatome Map: A Foundation for Understanding
The dermatome map depicts the distribution of sensory nerves, known as dermatomes, originating from specific spinal nerve roots. Each spinal nerve root serves a distinct region of the skin, forming a unique pattern across the body. The lumbar dermatomes, derived from the five lumbar spinal nerve roots (L1-L5), innervate the lower back, abdomen, hips, thighs, and parts of the legs.
The Significance of Lumbar Dermatomes
The lumbar dermatome map holds significant clinical importance, serving as a vital tool for:
- Diagnosing Neurological Conditions: When a patient experiences pain, numbness, or tingling in a specific area, the dermatome map helps pinpoint the potential source of the issue. For example, pain radiating down the front of the thigh could indicate compression of the L3 nerve root.
- Localizing Spinal Nerve Root Compression: Conditions like herniated discs, spinal stenosis, or nerve entrapment can compress spinal nerve roots, leading to specific sensory disturbances within the corresponding dermatomes.
- Identifying Spinal Cord Injuries: Damage to the spinal cord can disrupt the flow of sensory information, resulting in altered sensation within specific dermatomes. Mapping these changes can aid in understanding the extent and location of the spinal cord injury.
- Guiding Physical Therapy: Understanding the specific dermatomes involved in pain or weakness can help physical therapists design targeted exercises and treatments to address the underlying issue.
A Closer Look at Lumbar Dermatomes: Mapping the Pathways
Let’s examine the individual lumbar dermatomes and their associated areas:
- L1 Dermatome: This dermatome covers the skin of the lower abdomen, including the groin region.
- L2 Dermatome: The L2 dermatome extends from the upper thigh to the front of the hip.
- L3 Dermatome: This dermatome encompasses the anterior aspect of the thigh, including the knee joint.
- L4 Dermatome: The L4 dermatome covers the medial aspect of the leg, including the knee and inner ankle.
- L5 Dermatome: This dermatome encompasses the lateral aspect of the leg, including the foot, and extends to the big toe.
Beyond the Map: Understanding the Underlying Mechanisms
The dermatome map is a visual representation of the sensory pathways, but understanding the underlying mechanisms is crucial for comprehending its clinical significance.
- Sensory Nerves: Each dermatome is innervated by a specific spinal nerve root. These nerves carry sensory information from the skin, muscles, and joints back to the spinal cord and ultimately to the brain.
- Spinal Cord: The spinal cord acts as a conduit for sensory information, relaying it to the brain for processing.
- Brain: The brain interprets the sensory information received from the spinal cord, allowing us to perceive sensations like touch, temperature, and pain.
FAQs About the Lumbar Dermatome Map:
1. What causes changes in sensation within a specific dermatome?
Changes in sensation within a specific dermatome can be caused by various factors, including:
- Nerve Compression: Conditions like herniated discs, spinal stenosis, or nerve entrapment can compress spinal nerve roots, leading to sensory disturbances.
- Nerve Damage: Trauma, infection, or certain medical conditions can damage nerves, causing sensory loss or altered sensation within the corresponding dermatome.
- Spinal Cord Injury: Damage to the spinal cord can disrupt the flow of sensory information, leading to altered sensation within specific dermatomes.
- Peripheral Neuropathy: Conditions affecting the peripheral nerves, such as diabetes, can cause sensory disturbances in various dermatomes.
2. How is a dermatome map used in diagnosis?
A dermatome map is used in diagnosis by:
- Identifying the affected area: The location of sensory changes can help pinpoint the specific nerve root or spinal cord level involved.
- Differentiating between neurological and non-neurological causes: Changes in sensation within specific dermatomes suggest a neurological cause, while changes in sensation without a dermatomal pattern may indicate other issues.
- Monitoring the progression of neurological conditions: Changes in sensory distribution over time can indicate the progression or improvement of a neurological condition.
3. Can I use a dermatome map to self-diagnose?
While the dermatome map provides valuable information, self-diagnosis is not recommended. Consulting a medical professional is crucial for accurate diagnosis and appropriate treatment.
Tips for Understanding and Using the Lumbar Dermatome Map:
- Visualize the map: Familiarize yourself with the dermatome map and the areas covered by each lumbar dermatome.
- Consider the pattern of sensory changes: The distribution of sensory changes can provide valuable clues about the underlying cause.
- Consult a medical professional: If you experience any unexplained changes in sensation, seek medical advice for a proper diagnosis and treatment plan.
Conclusion
The lumbar dermatome map is a crucial tool for understanding the sensory pathways of the lower body. By providing a visual representation of the distribution of sensory nerves, it aids in diagnosing neurological conditions, localizing spinal nerve root compression, and guiding treatment strategies. While the map is a valuable resource for medical professionals, it is essential to remember that self-diagnosis is not recommended. Consulting a healthcare professional for any unexplained changes in sensation is crucial for accurate diagnosis and appropriate treatment.


Closure
Thus, we hope this article has provided valuable insights into Understanding the Lumbar Dermatome Map: A Guide to Sensory Pathways and Diagnosis. We appreciate your attention to our article. See you in our next article!